Point | Counterpoint – Lytics + Heparin or Heparin Alone for Intermediate Risk PE?
August 17, 2023
Written by Nickolas Srica
Spoon Feed
There is practice variation in the treatment of patients with intermediate-risk* pulmonary embolism (PE). The treatment threshold for which fibrinolytics should be added to standard anticoagulation in hemodynamically stable patients at risk for decompensation has been a focus of PE research for the last decade.
Let’s see how this one alte-plays out…(a little tPA pun for you)
This article provides a discourse on the treatment of intermediate-risk PE using a patient vignette. Two experts contended for treatment with either heparin + thrombolysis or heparin alone and were asked to defend their respective choices.
Clinical Case: A woman in her 30s with no significant medical history is diagnosed with a saddle PE and clinical signs of a proximal DVT. She was normotensive (BP = 116/80) but tachycardic (bpm = 122) and hypoxic (Sp02 = 92%), with evidence of right heart strain and elevated cardiac biomarkers.
The first expert (CK) advocates for low-dose thrombolysis, given the patient’s shock index >1, low bleeding risk, and elevated Bova Score showing a higher risk of complications and death. Citing the PEITHO trial, the expert argues, despite showing no overall mortality benefit, the trial showed a decreased risk of clinical deterioration in the younger (age < 75) subgroup.1 The expert also cites a meta-analysis showing a NNT of 51 to prevent death and a NNH of 176 for major bleeding in patients < 65 years of age.2 The second expert (TM) citing the same trial and others argues for heparin alone, citing an increased risk of catastrophic bleeding, no mortality benefit, and no reduction in the risk of long-term complications or prolonged hospitalization with thrombolytics, even in those with evidence of right heart strain.1,3
How will this change my practice?
There continues to be controversy surrounding the thrombolytic treatment threshold in patients with intermediate-risk PE. Several anticipated randomized controlled trials are currently investigating advanced PE treatments compared to anticoagulation alone.4-6 For now, we consider this decision on a case-by-case basis, with particular emphasis on impending clinical decompensation and bleeding risk before reaching for thrombolytics. And when in doubt, reach out to your friendly, neighborhood multidisciplinary PE response team early!
Peer reviewed and edited by Bo Stubblefield and Clay Smith
Source
Treatment of Intermediate-Risk Pulmonary Embolism. N Engl J Med. 2023 Jul 13;389(2):184-187. doi: 10.1056/NEJMclde2301330.
Another Spoonful
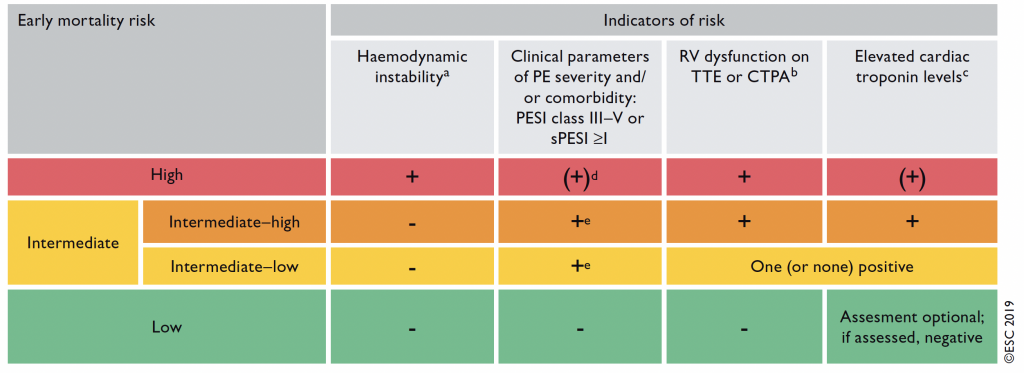
*What constitutes low, intermediate (low/high), and high risk? See this table.
Works Cited
- Meyer G, Vicaut E, Danays T, et al. Fibrinolysis for patients with intermediate-risk pulmonary embolism. N Engl J Med 2014;370:1402-11.
- Chatterjee S, Chakraborty A, Weinberg I, et al. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. Jama 2014;311:2414-21.
- Konstantinides SV, Vicaut E, Danays T, et al. Impact of Thrombolytic Therapy on the Long-Term Outcome of Intermediate-Risk Pulmonary Embolism. Journal of the American College of Cardiology 2017;69:1536-44.
- Sanchez O, Charles-Nelson A, Ageno W, et al. Reduced-Dose Intravenous Thrombolysis for Acute Intermediate-High-risk Pulmonary Embolism: Rationale and Design of the Pulmonary Embolism International THrOmbolysis (PEITHO)-3 trial. Thromb Haemost 2022;122:857-66.
- Ultrasound-facilitated, Catheter-directed, Thrombolysis in Intermediate-high Risk Pulmonary Embolism (HI-PEITHO). ClinicalTrials.gov Identifier: NCT04790370. (Accessed July 17th, 2023,
- Klok FA, Piazza G, Sharp ASP, et al. Ultrasound-facilitated, catheter-directed thrombolysis vs anticoagulation alone for acute intermediate-high-risk pulmonary embolism: Rationale and design of the HI-PEITHO study. Am Heart J 2022;251:43-53.

